The young woman trips on an uneven sidewalk, recovers smoothly and resumes texting. The older woman encounters the same perturbation and crashes.
My colleagues and I have been trying to identify the key neuromuscular attributes responsible for successful response to perturbation in our clinical practice for quite some time. We have been particularly interested in older people with diabetic neuropathy since this population is advised to walk for exercise, and yet commonly falls. Traditionally, we looked at hip muscle strength generation and ankle proprioceptive precision to explain unipedal stance time and gait speed. However, against our expectations these neuromuscular attributes did not predict lateral gait variability or the few major injuries sustained by our study participants.
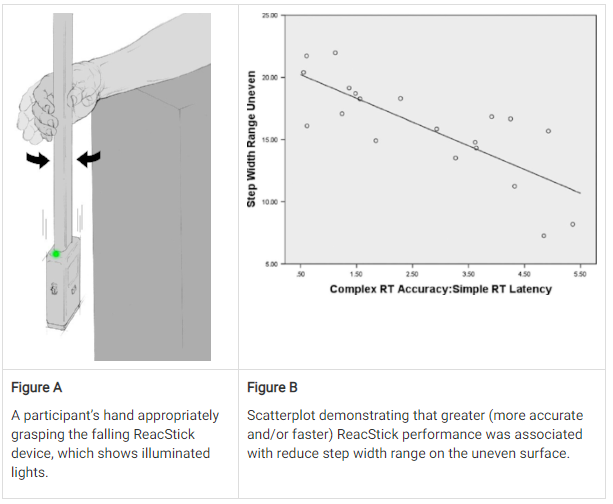
Since the neuromuscular variables were unrevealing, I looked for relationships between step width variability and Simple Reaction Time and Complex Reaction Accuracy using our ReacStick device (see Figure). The ReacStick is a rigid, lightweight rod with a rectangular box at one end. To determine SRT the participant sits with an open hand around the box, and as quickly as possible catches the suspended device, which is dropped at random intervals by the examiner. When determining Complex Reaction Accuracy, the participant catches the device solely when the LED lights illuminate on the housing when dropped during 50% of the trials. If the LED lights do not illuminate then the participant is asked to let the device fall to the floor, requiring a Jedi-quick decision as the ReacStick hits the floor in about 400 msec (an interval similar to the swing phase of gait).
Our results showed that the ratio of Complex Reaction Accuracy to Simple Reaction Time, which rewards accuracy and/or quick reaction, was strongly and inversely associated with uneven surface gait variability in participants suffering from neuropathy (R2 = .61). Further, the participants with major fall-related injuries appeared less accurate and slower than those without. The effects were less prominent in the older participants without neuropathy.
The results suggest that people with lower limb neuromuscular impairment rely on neurocognitive speed, as determined by the ability to perceive a stimulus and quickly inhibit a motor response, to maintain postural control when navigating an uneven surface and, possibly, to prevent severe injury in the event of a fall.
The texting young woman likely has a quicker brain… which may be clinically detectable.
Publication
Richardson JK, Eckner JT, Allet LA, Kim H, Ashton-Miller JA. Complex and simple clinical reaction times are associated with gait, balance, and major fall injury in older subjects with diabetic peripheral neuropathy. Am J Phys Med Rehabil 2017;96:8-16.
About the Author

Dr. Richardson
Professor of Physical Medicine/Rehabilitation at the University of Michigan
Dr. Richardson is a Professor of Physical Medicine/Rehabilitation at the University of Michigan where he directs the Electrodiagnostic Laboratory and is actively engaged in patient care and teaching.His primary research interests include investigating the influence of peripheral nerve function on gait/balance, and translating insights from the biomechanics laboratory into the clinical realm.
Copyright
© 2018 by the author. Except as otherwise noted, the ISPGR blog, including its text and figures, is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by-sa/4.0/legalcode.
ISPGR blog (ISSN 2561-4703)
Are you interested in writing a blog post for the ISPGR website? If so, please email the ISGPR Secretariat with the following information:
- First and Last Name
- Institution/Affiliation
- Paper you will be referencing

